Can you exercise with POTS? Yes, with careful planning and the right approach, you can absolutely exercise with Postural Orthostatic Tachycardia Syndrome (POTS). The key is to find safe exercise for POTS, focusing on low impact exercise and POTS exercise modifications to gradually build strength and stamina without triggering symptoms. This guide will explore effective POTS exercise strategies to help you manage fatigue and improve your quality of life through movement.
Living with POTS presents unique challenges, especially when it comes to physical activity. The autonomic dysfunction that defines POTS can lead to a range of debilitating symptoms, including dizziness, fatigue, heart palpitations, and brain fog. For many, the thought of exercise can seem daunting, if not impossible. However, consistent and appropriate movement is crucial for managing POTS and improving overall well-being. It’s about finding what works for your body and adapting it.
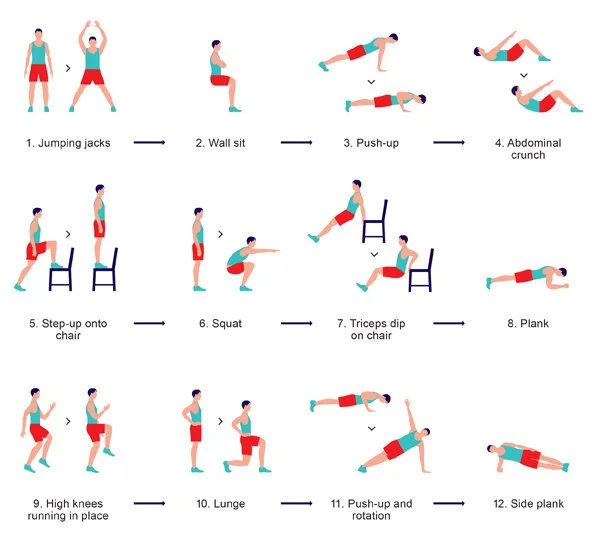
Image Source: images.squarespace-cdn.com
Embracing Movement: The Foundation of POTS Exercise
Exercise, when approached correctly, can be a powerful tool in managing POTS. It can help improve cardiovascular health, strengthen muscles, increase blood volume, and even reduce the severity of symptoms over time. The goal isn’t to push through pain or exhaustion, but to build a sustainable fitness routine that supports your body’s needs.
Why Exercise Matters for POTS
- Increased Blood Volume: Exercise can encourage your body to produce more blood, which is essential for individuals with POTS who often have reduced blood volume.
- Improved Cardiovascular Function: Regular, gentle exercise can strengthen your heart and improve its efficiency in pumping blood.
- Enhanced Muscle Strength: Stronger muscles, especially in the legs, can help with blood return to the heart.
- Better Autonomic Regulation: Consistent movement can help retrain your autonomic nervous system, potentially leading to fewer dysautonomia symptoms.
- Reduced Fatigue: While it seems counterintuitive, moderate exercise can actually combat the overwhelming fatigue associated with POTS.
- Mood Enhancement: Physical activity releases endorphins, which can improve mood and reduce feelings of anxiety and depression that can co-occur with chronic illness.
Designing Your POTS-Friendly Workout Plan
The cornerstone of exercising with POTS is graded exercise therapy (GET) POTS. This approach involves starting with very low-intensity activities and gradually increasing the duration, frequency, and intensity as your body tolerates it. It’s a marathon, not a sprint, and patience is your greatest ally.
Key Principles for POTS Exercise
- Listen to Your Body: This is paramount. If you feel symptoms worsening, stop or reduce the intensity. Don’t push through dizziness, nausea, or extreme fatigue.
- Stay Hydrated: Drink plenty of fluids, especially water, before, during, and after exercise. Electrolyte drinks can also be beneficial.
- Increase Salt Intake (with doctor’s advice): For some with POTS, a slightly higher sodium intake can help increase blood volume. Always consult your doctor before making dietary changes.
- Wear Compression Garments: Abdominal binders and thigh-high compression stockings can help improve blood flow back to the heart.
- Avoid Hot Environments: Heat can exacerbate POTS symptoms. Exercise in cool, well-ventilated areas.
- Gradual Progression: Start slow and build up. It might take weeks or months to reach a level of activity that feels challenging but manageable.
- Consistency is Key: Aim for regular movement, even if it’s just for a few minutes each day.
- Prioritize Lying or Seated Positions: Many exercises can be modified to be done lying down or seated, which can help manage orthostatic intolerance.
Types of Exercise for POTS Management
Focusing on low impact exercise is generally recommended for POTS. These activities put less stress on your joints and cardiovascular system, making them more tolerable.
1. Cardiovascular Exercise
Cardio is essential, but it needs to be approached cautiously. The goal is to build endurance without overtaxing your system.
Lie-Down or Seated Cardio
- Recumbent Cycling: A stationary bike where you sit in a reclined position is excellent. It reduces the gravitational pull on blood, making it a fantastic POTS friendly workout. Start with 5-10 minutes at a very low resistance.
- Arm Cycling (Ergometer): Similar to a stationary bike but for your arms. This is a great way to get your heart rate up without significant upright exercise POTS strain.
- Seated Aerobics: Many online videos offer seated aerobic routines that are gentle and effective.
- Swimming or Water Aerobics: The buoyancy of water supports your body, reducing the feeling of strain. The cool temperature can also be beneficial. Water walking is a good starting point.
Gradual Upright Cardio
Once you can tolerate seated or lying down cardio well, you can slowly introduce upright activities.
- Walking: Begin with short walks (5-10 minutes) on flat surfaces. Increase duration before increasing pace or incline.
- Elliptical Trainer: This offers a low-impact cardio workout that can be gentler than running or jogging.
- Rowing Machine: Can be a good option if done with proper form and controlled intensity, as it involves both upper and lower body.
2. Strength Training
Building muscle helps support your body and can improve blood circulation. Focus on controlled movements and lighter weights or resistance bands.
Key Strength Training Considerations
- Avoid Valsalva Maneuver: Do not hold your breath during exertion, as this can spike blood pressure and worsen POTS symptoms. Exhale during the effort phase of the exercise.
- Focus on Compound Movements: Exercises that work multiple muscle groups are efficient.
- Progressive Overload: Gradually increase the resistance, repetitions, or sets as you get stronger.
Effective Strength Exercises for POTS
- Chair Squats: Stand up from a chair and sit back down slowly and controlled.
- Wall Sits: Lean against a wall with your feet shoulder-width apart, sliding down until your knees are bent at a 90-degree angle. Hold for a short period and gradually increase.
- Bridges: Lie on your back with knees bent and feet flat on the floor. Lift your hips off the ground, squeezing your glutes.
- Bicep Curls & Tricep Extensions: Use light dumbbells or resistance bands. Perform these seated or lying down.
- Core Strengthening: Planks (start on knees if needed), bird-dog, and dead bug exercises can be done lying down.
- Calf Raises: Stand and rise up onto your toes. This is particularly beneficial for improving blood return from the legs.
3. Flexibility and Balance
Flexibility exercises and balance training can also be beneficial and are generally well-tolerated.
- Stretching: Gentle static stretches for major muscle groups can improve flexibility and reduce muscle tension. Hold stretches for 20-30 seconds.
- Yoga and Pilates (Modified): These can be excellent POTS exercise modifications. Focus on gentle, restorative styles. Many poses can be done lying down or seated. Avoid inversions or poses that significantly change your head position rapidly. Look for POTS friendly workouts that emphasize core strength and controlled movements.
- Tai Chi: This slow, flowing martial art is excellent for balance, coordination, and mindfulness.
- Vestibular Rehabilitation POTS: For those experiencing dizziness or balance issues, specific vestibular exercises can be very helpful. These often involve controlled head movements and visual focus exercises, but should be initiated under the guidance of a physical therapist or healthcare professional.
Sample Gradual Exercise Progression (GET POTS)
This is a sample progression. Your personal journey may be faster or slower, and that’s perfectly okay. Always consult with your doctor or a physical therapist experienced with POTS.
Phase 1: Acclimation (Weeks 1-4)
- Frequency: 3-4 days per week.
- Activity:
- Recumbent cycling or arm ergometer: 10-15 minutes at a very low resistance. Focus on maintaining a steady rhythm.
- Gentle seated stretching: 10 minutes daily.
- Optional: 5-10 minute slow walk on flat ground, if tolerated.
- Focus: Building a habit, preventing symptom flares, and gradually increasing tolerance to movement.
Phase 2: Building Endurance (Weeks 5-12)
- Frequency: 4-5 days per week.
- Activity:
- Recumbent cycling/arm ergometer: Increase duration to 20-30 minutes. You can slowly increase resistance slightly if tolerated.
- Strength training: 2-3 days per week, focusing on bodyweight or light resistance bands. 1-2 sets of 10-15 repetitions. Exercises like chair squats, bridges, and seated bicep curls.
- Walking: Gradually increase duration to 15-20 minutes. Maintain a comfortable pace.
- Focus: Increasing cardiovascular stamina and muscle strength.
Phase 3: Increasing Intensity & Variety (Months 3-6)
- Frequency: 5 days per week.
- Activity:
- Cardio: 30-40 minutes. You can now consider adding very light incline to walking, or slightly higher resistance on the bike, IF symptoms allow.
- Strength training: 3 days per week. Increase resistance slightly or add a third set. Introduce new exercises like wall sits or seated rows.
- Consider introducing other low impact exercise like water aerobics or gentle yoga.
- Focus: Further improving cardiovascular fitness and strength, exploring different types of POTS exercise modifications.
Phase 4: Maintenance and Further Progression (Ongoing)
- Frequency: 5-6 days per week.
- Activity: Continue with a balanced routine of cardio, strength, and flexibility. You can gradually increase the intensity or duration of workouts as your body continues to adapt.
- Focus: Maintaining fitness levels, continuing to challenge the body within safe limits, and potentially trying new activities that are still POTS friendly workouts.
Specific Exercise Modifications for POTS
The beauty of POTS exercise strategies is their adaptability. Here are some common POTS exercise modifications to help you succeed:
- Avoid Prolonged Standing: If an exercise requires standing, see if it can be done seated or lying down. For activities like walking, take frequent breaks to sit or lean.
- Keep Head Below Heart: Whenever possible, perform exercises in a horizontal or reclined position. This reduces the strain on your cardiovascular system.
- Use a Heart Rate Monitor: Keep your heart rate within a target zone that is safe for you. This often means staying at a lower percentage of your maximum heart rate than a healthy individual without POTS might aim for. Your doctor can help determine this zone.
- Hydration and Electrolytes: Keep water and electrolyte-rich drinks readily available. Sip them frequently throughout your workout.
- Cool Down Properly: A gradual cool-down is essential. Don’t stop abruptly. Spend 5-10 minutes lowering your heart rate slowly.
- Listen to Your Symptoms: Dizziness, lightheadedness, nausea, palpitations, or significant fatigue are signals to stop or reduce intensity. Don’t ignore them.
- Abdominal Binder/Compression Garments: Wearing these during exercise can significantly help with symptom management.
When to Seek Professional Guidance
It’s highly recommended to work with professionals who are familiar with autonomic dysfunction and POTS.
Who Should You Consult?
- Your Doctor: Essential for diagnosis and to get clearance for exercise. They can help identify any co-occurring conditions that might affect your exercise plan.
- Physical Therapist (PT): A PT experienced with POTS or dysautonomia can create a personalized graded exercise therapy POTS program tailored to your specific needs and limitations. They can also help with vestibular rehabilitation POTS if that’s a concern.
- Exercise Physiologist: Similar to a PT, an exercise physiologist can design safe and effective exercise programs.
- Registered Dietitian: Can help you optimize hydration and electrolyte intake.
Common Challenges and How to Overcome Them
- Fear of Symptom Flare-ups: Start extremely slowly. Celebrate small victories. Recognize that a setback doesn’t mean failure; it means adjusting the plan.
- Profound Fatigue: Break exercise into smaller, more frequent sessions throughout the day. Even 5 minutes of movement counts.
- Brain Fog: Keep your exercise plan simple and written down. Use timers and visual cues.
- Heat Intolerance: Exercise indoors in a cool environment or during cooler parts of the day.
- Orthostatic Intolerance: Prioritize lying or seated exercises. Use compression. Stay hydrated.
Frequently Asked Questions (FAQ)
What is the best type of exercise for POTS?
The best type of exercise for POTS is typically low impact exercise performed in lying or seated positions. Examples include recumbent cycling, swimming, water aerobics, and seated strength training. Gradual progression using graded exercise therapy POTS principles is crucial.
How often should I exercise with POTS?
Aim for consistency. Starting with 3-4 days a week is a good goal. As you progress, you might move to 4-5 days a week, focusing on POTS exercise strategies that prioritize symptom management over high intensity.
Can I do upright exercise with POTS?
Yes, but with extreme caution and only after establishing tolerance for lying or seated exercises. Start with very short durations and gradually increase. Walking on flat surfaces is often the first upright exercise POTS to try. Always use POTS exercise modifications like compression garments and stay hydrated.
How do I know if I’m pushing too hard?
Listen to your body. Symptoms like increased dizziness, lightheadedness, nausea, palpitations, shortness of breath beyond normal exertion, or a significant increase in fatigue are signs you need to stop or reduce intensity.
Will exercise make my POTS worse?
If done incorrectly or too intensely, yes, exercise can worsen POTS symptoms. However, when done gradually and with appropriate POTS exercise modifications and safe exercise for POTS principles, it is one of the most effective management strategies.
How long does it take to see improvements from exercise with POTS?
Improvements can vary greatly from person to person. Some may notice small benefits within weeks, while others may take months to feel significant changes. Consistency and patience are key.
Conclusion
Navigating exercise with POTS requires a mindful, patient, and adaptive approach. By focusing on safe exercise for POTS, embracing low impact exercise, and implementing smart POTS exercise strategies, you can gradually build strength, improve your cardiovascular health, and effectively manage fatigue. Remember that every step forward, no matter how small, is a victory. With the right POTS exercise modifications and a commitment to listening to your body, you can indeed beat fatigue and move towards a more active and fulfilling life. Consulting with healthcare professionals experienced in autonomic dysfunction exercise and vestibular rehabilitation POTS is highly recommended to create a personalized and effective plan.
