Image Source: tomenybest.com
Herniated Disc: Can I Exercise Safely? Your Pain-Free Guide
Yes, you can exercise with a herniated disc, but safely and with careful consideration. The key is to choose the right exercises, modify them appropriately, and listen to your body. While movement is often beneficial, certain activities can worsen a herniated disc, so a tailored approach is essential. This guide will help you navigate the world of exercise with a herniated disc, ensuring you can stay active and work towards a pain-free life.
Deciphering Herniated Discs and Their Impact on Movement
A herniated disc, often referred to as a slipped or ruptured disc, occurs when the soft, jelly-like center of an intervertebral disc pushes through a tear in its tougher outer layer. This condition, also known as a herniated nucleus pulposus, can cause significant back pain and other symptoms if the protruding material presses on nearby nerves. Common culprits include the disc bulge, which is a less severe form where the disc pushes outward without a full rupture.
The spine is a complex structure made of vertebrae separated by discs. These discs act as shock absorbers. When a disc herniates, the inner material can bulge or leak out, potentially irritating or compressing spinal nerves. This nerve compression can lead to a range of issues, including:
- Sciatica: Pain that radiates down the leg due to compression of the sciatic nerve.
- Numbness and Tingling: A pins-and-needles sensation in the affected limb.
- Weakness: Difficulty moving certain muscles in the arms or legs.
- Localized Pain: Discomfort in the back or neck, depending on the herniation’s location.
It’s crucial to remember that the severity of symptoms doesn’t always correlate with the size of the herniation. Some people with significant disc herniations have no pain, while others with smaller ones experience intense discomfort.
Why Movement Matters: The Benefits of Exercise with a Herniated Disc
Contrary to what some may believe, rest is not always the best medicine for a herniated disc. While aggressive or high-impact activities should be avoided, gentle and targeted exercise offers numerous advantages:
- Strengthens Supporting Muscles: Exercise, particularly focusing on core strengthening, helps build stronger muscles around the spine. These muscles act like a natural brace, supporting the vertebrae and reducing stress on the discs.
- Improves Flexibility and Range of Motion: Gentle stretching can help relieve muscle tension and improve the spine’s mobility, reducing stiffness often associated with back pain.
- Increases Blood Flow: Movement promotes circulation, which can aid in the healing process by delivering nutrients and oxygen to the affected area.
- Reduces Pain: Many exercises, when performed correctly, can alleviate pressure on the nerves and reduce pain signals.
- Prevents Future Injury: By strengthening the core and improving posture, regular exercise can help prevent recurrence of disc problems.
- Boosts Mood and Reduces Stress: Chronic pain can take a toll on mental well-being. Exercise is a natural mood booster and stress reliever.
Essential Considerations Before You Start Exercising
Before embarking on any exercise program for a herniated disc, it is paramount to consult with a healthcare professional. This usually includes your doctor and potentially a physical therapist. They can:
- Diagnose the specific nature of your herniation: Different types of herniations and their locations require different approaches.
- Assess your current condition: They can determine your pain levels, flexibility, and strength.
- Recommend appropriate exercises: They will guide you on which disc herniation exercises are safe and effective for you.
- Advise on modifications: They can show you how to adapt exercises to suit your needs.
- Set realistic goals: They will help you create a progression plan.
Ignoring this step can lead to further injury or exacerbation of your condition.
Red Flags: When to Stop and Seek Medical Advice
It’s vital to listen to your body and recognize warning signs. Stop exercising immediately and contact your doctor if you experience any of the following:
- Increased or sharp pain during or after exercise.
- Numbness or tingling that worsens or spreads.
- Loss of bladder or bowel control (this is a medical emergency).
- Severe weakness in your legs or arms.
- Pain that radiates further down your leg than before.
Safe and Effective Exercises for Herniated Discs
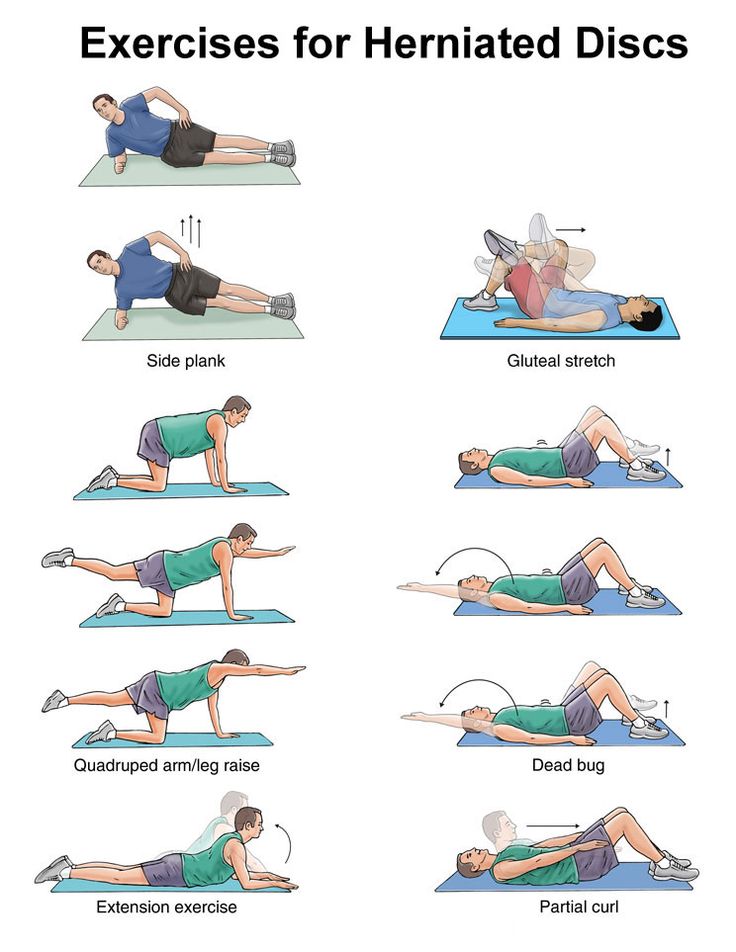
The goal is to strengthen and stabilize the spine without putting undue pressure on the affected disc. Focus on exercises that promote controlled movement and muscle engagement.
Core Strengthening Exercises
A strong core is the foundation for a healthy spine. These exercises help stabilize the trunk, reducing the load on the intervertebral discs.
1. Pelvic Tilts
- How to: Lie on your back with knees bent and feet flat on the floor. Gently flatten your lower back against the floor by tightening your abdominal muscles and tilting your pelvis upward. Hold for a few seconds, then relax.
- Why it helps: This engages the deep abdominal muscles and is a gentle way to activate the core.
2. Bird-Dog
- How to: Start on your hands and knees, with your hands directly under your shoulders and knees under your hips. Keep your back straight and core engaged. Slowly extend your right arm straight forward and your left leg straight back, keeping your hips level. Hold for a few seconds, then return to the starting position. Repeat on the other side.
- Why it helps: This exercise improves core stability and balance while minimizing spinal rotation.
3. Modified Plank
- How to: Begin on your hands and knees. Lower your forearms to the floor, keeping your elbows directly under your shoulders. Extend your legs back, resting on your knees. Keep your body in a straight line from head to knees, engaging your core. Hold for 20-30 seconds.
- Why it helps: This is a less intense version of the standard plank that still effectively works the core muscles. As you get stronger, you can progress to a full plank on your toes.
4. Bridge Pose
- How to: Lie on your back with knees bent, feet flat on the floor hip-width apart, and arms by your sides. Engage your glutes and lift your hips off the floor, creating a straight line from your shoulders to your knees. Hold for a few seconds, then slowly lower back down.
- Why it helps: This strengthens the glutes and hamstrings, which are essential for supporting the lower back.
Gentle Stretching and Mobility Exercises
Stretching can improve flexibility and reduce muscle spasms, which often accompany a herniated disc.
1. Knee-to-Chest Stretch
- How to: Lie on your back with knees bent. Gently bring one knee towards your chest, using your hands to assist if needed. Hold for 20-30 seconds, breathing deeply. Repeat with the other leg. You can also try bringing both knees to your chest simultaneously.
- Why it helps: This stretches the lower back and glutes, relieving tension.
2. Cat-Cow Stretch
- How to: Start on your hands and knees. As you inhale, drop your belly towards the floor and lift your head and tailbone (cow pose). As you exhale, round your spine towards the ceiling, tucking your chin to your chest (cat pose). Move slowly and rhythmically between the two poses.
- Why it helps: This gently mobilizes the spine and increases awareness of spinal movement.
3. Seated Spinal Twist
- How to: Sit on the floor with legs extended. Bend your right knee and place your right foot flat on the floor outside your left thigh. Place your left elbow on the outside of your right knee and gently twist your torso to the right, looking over your right shoulder. Hold for 20-30 seconds, then repeat on the other side.
- Why it helps: This stretch improves spinal mobility and can relieve tension in the back muscles. Ensure the twist is gentle and controlled.
Low-Impact Aerobic Exercise
Aerobic exercise is crucial for overall health and can help with weight management, which is important for reducing stress on the spine.
1. Walking
- How to: Start with short walks on a flat surface. Gradually increase the duration and intensity as your pain allows. Good posture is key.
- Why it helps: Walking is a low-impact activity that improves cardiovascular health and strengthens leg muscles without jarring the spine.
2. Swimming or Water Aerobics
- How to: The buoyancy of water reduces stress on the spine, making it an ideal environment for exercise. Focus on gentle strokes like the breaststroke or backstroke. Avoid the butterfly stroke if it aggravates your pain.
- Why it helps: Water provides resistance for strengthening and support for movement, making it very forgiving on the back.
3. Stationary Cycling
- How to: Adjust the bike seat to a comfortable height to maintain a slight bend in your knees when the pedal is at its lowest point. Start with low resistance and gradually increase as tolerated.
- Why it helps: Cycling is a good cardiovascular workout that can be done without impact. Ensure your posture is upright to avoid rounding your back.
Exercises to Approach with Caution or Avoid
Certain movements can place excessive strain on a herniated disc and should be avoided or performed with extreme caution, ideally under the guidance of a physical therapist.
- Heavy Lifting: Especially lifting with your back instead of your legs.
- High-Impact Activities: Running, jumping, aerobics with jumping.
- Exercises involving significant spinal flexion: Crunches, sit-ups, toe touches.
- Exercises involving forceful twisting: Certain rotational movements.
- Exercises that cause pain: If an exercise hurts, stop immediately.
The Role of Physical Therapy in Herniated Disc Treatment
Physical therapy is a cornerstone of herniated disc treatment. A physical therapist is trained to assess your specific condition and develop a personalized exercise program. They can employ various techniques, including:
Spinal Decompression Techniques
Spinal decompression aims to reduce pressure on the spinal nerves. This can be achieved through:
- Mechanical traction: Using a machine to gently stretch the spine.
- Manual traction: A therapist uses their hands to gently pull on the spine.
- Specific exercises: Certain movements can create a mild decompression effect.
Therapeutic Exercise Progression
Physical therapists will guide you through a carefully planned exercise progression:
- Phase 1: Pain Relief and Gentle Movement: Focus on reducing inflammation and pain with modalities like ice, heat, and gentle mobilization exercises.
- Phase 2: Core Stabilization and Strength: Introduce exercises to build core strength and improve posture, like those mentioned above.
- Phase 3: Functional Movement and Endurance: Progress to exercises that mimic daily activities and improve overall fitness.
- Phase 4: Maintenance and Prevention: Establish a long-term exercise routine to maintain spinal health and prevent recurrence.
Lifestyle Modifications for Managing Herniated Discs
Beyond exercise, several lifestyle adjustments can significantly contribute to managing a herniated disc and preventing further issues:
- Maintain a Healthy Weight: Excess weight puts additional strain on your spine.
- Practice Good Posture: Whether sitting, standing, or lifting, proper posture is crucial.
- Ergonomics: Adjust your workspace to support good posture. Use lumbar support when sitting for extended periods.
- Proper Lifting Techniques: Always bend your knees and keep your back straight when lifting.
- Avoid Prolonged Sitting: Get up and move around every 30-60 minutes.
- Quit Smoking: Smoking can negatively impact disc health and slow healing.
Can I Exercise with Degenerative Disc Disease?
Yes, individuals with degenerative disc disease can also benefit from exercise. Degenerative disc disease refers to the breakdown of discs over time, which can be a contributing factor to or consequence of herniation. Similar principles apply:
- Focus on low-impact exercises.
- Prioritize core strengthening.
- Maintain flexibility.
- Listen to your body and avoid aggravating activities.
A physical therapist can help tailor a program that addresses the specific changes associated with degenerative disc disease.
Frequently Asked Questions (FAQ)
Q1: How soon can I start exercising after a herniated disc?
A1: This varies greatly depending on the severity of the herniation and your symptoms. Typically, after the initial acute pain subsides and with your doctor’s or physical therapist’s approval, gentle exercises can begin. It’s crucial to start slowly and gradually.
Q2: Will exercise make my herniated disc worse?
A2: If you do the wrong exercises or perform them with poor form, it can worsen your condition. However, the right exercises, done correctly and progressively, are essential for recovery and preventing future problems. Always follow the guidance of a healthcare professional.
Q3: What are the best exercises for sciatica relief?
A3: Exercises that gently stretch the piriformis muscle and strengthen the core are often beneficial for sciatica relief. Examples include knee-to-chest stretches, piriformis stretches, and gentle spinal mobilization exercises. Again, consult a professional for personalized advice.
Q4: Is yoga or Pilates good for a herniated disc?
A4: Yes, certain types of yoga and Pilates can be highly beneficial, provided they are modified for your condition. Gentle, restorative yoga and Pilates focusing on core strength and controlled movements are usually recommended. Avoid poses that involve deep forward bends, extreme twists, or inversions initially. Always inform your instructor about your herniated disc.
Q5: How long does it take to recover from a herniated disc?
A5: Recovery timelines vary widely. Many people experience significant improvement within weeks to months with conservative treatment, including physical therapy and exercise. However, some may have ongoing issues, especially with more severe herniations or if treatment is delayed.
Q6: Can I do strength training with weights if I have a herniated disc?
A6: Yes, but with significant caution and guidance. Focus on lighter weights with proper form, prioritize compound movements that engage the core, and avoid exercises that put direct pressure on the spine. Machines can sometimes be safer than free weights as they guide movement. Always get clearance and advice from your doctor or physical therapist.
Conclusion: Your Path to a More Active and Pain-Free Life
Living with a herniated disc doesn’t mean giving up an active lifestyle. By approaching exercise with knowledge, caution, and professional guidance, you can strengthen your body, reduce pain, and improve your overall quality of life. Remember that consistency and patience are key. Work with your healthcare team to develop a personalized exercise plan, listen to your body, and celebrate your progress on the path to a pain-free existence. The journey may require adjustments, but the rewards of regaining your ability to move freely are well worth the effort.
