If you have a blood clot in your leg, can you exercise? Generally, yes, but with significant caution and doctor approval. Exercise with a blood clot in your leg (Deep Vein Thrombosis or DVT) is a complex issue with potential risks and rewards. It’s crucial to consult your healthcare provider before engaging in any physical activity. This article explores the nuances of exercising with a blood clot in your leg, focusing on safety, potential benefits, and what to expect during the recovery process.
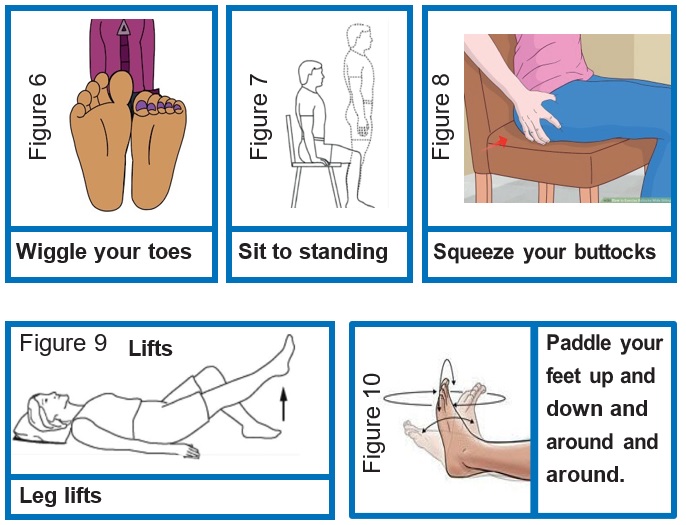
Image Source: www.buckshealthcare.nhs.uk
Decoding the Risks of Exercising with a Blood Clot
Exercising with a blood clot in your leg, also known as deep vein thrombosis (DVT), carries specific risks that must be carefully managed. The primary concern is the potential for the clot to dislodge and travel to other parts of the body, most dangerously to the lungs, causing a pulmonary embolism (PE). PE is a serious medical emergency.
Dislodgement and Pulmonary Embolism
A blood clot, typically a deep vein thrombosis (DVT), forms when blood pools and coagulates within a deep vein, most commonly in the leg. This stagnant blood can create a thrombus, a semi-solid mass. If this thrombus breaks free from the vein wall, it can travel through the bloodstream.
- Mechanism of Dislodgement: Certain movements, especially those involving sudden or forceful contractions of leg muscles, can potentially disrupt the clot’s attachment to the vein wall. This is particularly concerning in the early stages of DVT when the clot may be less firmly anchored.
- Journey to the Lungs: Once dislodged, the clot fragment travels through the venous system, eventually reaching the heart and then the lungs. In the lungs, it can lodge in an artery, blocking blood flow. This blockage is a pulmonary embolism (PE).
- Symptoms of PE: Symptoms of PE can include sudden shortness of breath, chest pain that worsens with deep breathing or coughing, rapid heart rate, coughing up blood, lightheadedness, or even fainting. Immediate medical attention is vital if these symptoms occur.
Increased Leg Pain with Blood Clot
Another significant risk is exacerbating the existing leg pain with blood clot. DVT often causes discomfort, swelling, redness, and warmth in the affected leg. Exercise, particularly if it involves high impact or extensive use of the leg muscles, can increase inflammation and put additional strain on the already compromised vein.
- Inflammation: Physical activity can sometimes increase inflammation in the affected limb, leading to more pronounced leg pain.
- Pressure on Veins: Certain exercises might increase pressure within the leg veins, potentially worsening the discomfort associated with the clot.
Risk of Bleeding from Anticoagulant Therapy
Individuals diagnosed with a blood clot are typically prescribed anticoagulant medication, often referred to as blood thinners. While essential for preventing further clot formation and managing existing ones, these medications increase the risk of bleeding.
- Impact of Exercise on Bleeding: Strenuous exercise, especially activities that carry a risk of falls or injuries, can lead to bruising or more significant bleeding if a cut or scrape occurs while on anticoagulant therapy.
- Severity of Bleeding: Even minor injuries can result in prolonged bleeding or hematoma formation (blood collecting outside of blood vessels) when taking blood thinners.
The Potential Rewards of Judicious Exercise
Despite the risks, carefully considered physical activity can offer significant benefits for individuals managing a blood clot. The key is to approach exercise strategically and under medical guidance.
Improving Circulation and Preventing Future Clots
Regular, low-impact exercise can help improve overall blood circulation, which is fundamental in both the management of current clots and the prevention of future ones.
- Enhanced Blood Flow: Muscle contractions during exercise act as a pump, aiding the return of blood to the heart. This improved venous return can help prevent blood from pooling in the legs.
- Endothelial Function: Exercise can improve the health of the endothelium, the inner lining of blood vessels. Healthy endothelium plays a role in preventing clot formation.
- Blood Clot Prevention: By promoting good circulation and vascular health, regular physical activity is a cornerstone of blood clot prevention strategies for those at risk.
Accelerating Recovery and Post-Clot Leg Care
Once the initial acute phase of DVT has passed and anticoagulant therapy is stable, controlled physical activity can be beneficial for post-clot leg care and long-term recovery.
- Reducing Post-Thrombotic Syndrome (PTS): PTS is a common complication of DVT, characterized by chronic leg pain, swelling, skin changes, and potentially ulcers. Regular exercise, particularly walking, can help reduce the severity and incidence of PTS.
- Restoring Muscle Strength: Prolonged immobility due to DVT can lead to muscle weakness. Gradual exercise helps rebuild strength and improve leg function.
- Managing Swelling: Gentle movements can help pump lymphatic fluid and reduce swelling that often persists after a DVT.
Enhancing Overall Well-being
The psychological benefits of exercise are also important. Managing a chronic or potentially life-threatening condition like DVT can be stressful. Physical activity is a proven mood booster and can help combat feelings of anxiety and depression.
- Mood Improvement: Exercise releases endorphins, which have mood-lifting effects.
- Stress Reduction: Physical activity provides an outlet for stress and can improve sleep quality.
- Increased Energy Levels: Counterintuitively, regular exercise can combat fatigue and increase overall energy.
Exercising with DVT: A Step-by-Step Approach
When considering exercise with a blood clot in your leg, a cautious, phased approach is essential. Always prioritize medical advice.
Step 1: Consult Your Healthcare Provider
This is the most critical step. Before undertaking any form of exercise, discuss your plans with your doctor or specialist.
- Assess Your Condition: Your doctor will evaluate the size and location of the clot, your overall health, and the stability of your anticoagulant therapy.
- Personalized Recommendations: They can provide specific recommendations tailored to your individual situation, including what types of exercises are safe and what to avoid.
- Medication Review: They will ensure your anticoagulant dosage is appropriate and discuss any potential interactions with exercise.
Step 2: Understand the Symptoms of Blood Clot in Leg
Recognizing the signs of a blood clot in your leg is crucial, not just for diagnosis but also for knowing when to stop exercising or seek medical help.
- Common Symptoms:
- Swelling in the affected leg (often one leg).
- Pain or tenderness in the leg, which may feel like a cramp or soreness.
- Redness or discoloration of the skin on the leg.
- Warmth in the leg compared to the other leg.
- Leg pain that worsens when standing or walking.
Step 3: Focus on Low-Impact Activities
The goal is to promote circulation without putting excessive stress on the affected leg or risking clot dislodgement.
Safe Exercise Options:
- Walking: This is often the cornerstone of exercise for DVT patients. Start with short, slow walks and gradually increase duration and pace as tolerated.
- Frequency: Daily if possible.
- Intensity: Light to moderate.
- Duration: Begin with 10-15 minutes, building up to 30 minutes or more.
- Cycling (Stationary or Outdoor): Gentle cycling can be excellent for leg circulation. Ensure a comfortable seat height and resistance.
- Frequency: 3-5 times per week.
- Intensity: Light to moderate.
- Duration: 20-30 minutes.
- Swimming or Water Aerobics: The buoyancy of water reduces stress on the joints and limbs. Water pressure can also help with swelling.
- Frequency: 2-3 times per week.
- Intensity: Moderate.
- Duration: 30-45 minutes.
- Gentle Yoga or Tai Chi: These can improve flexibility, balance, and circulation through slow, controlled movements.
- Frequency: 1-2 times per week.
- Intensity: Gentle.
- Duration: 30-60 minutes.
Step 4: Gradual Progression and Monitoring
Listen to your body and progress slowly.
- Start Slow: Begin with shorter durations and lower intensity.
- Increase Gradually: Over days and weeks, slowly increase the length of your sessions or the intensity.
- Monitor Symptoms: Pay close attention to any increase in leg pain, swelling, or other DVT symptoms. If you experience any of these, stop exercising and consult your doctor.
- Hydration: Drink plenty of water before, during, and after exercise.
Step 5: What to Avoid
Certain types of exercise should be avoided, especially in the initial stages of DVT management.
High-Risk Exercises:
- High-Impact Activities: Running, jumping, and sports involving quick stops and starts can put excessive strain on the legs.
- Heavy Weightlifting: Lifting very heavy weights, particularly those that involve straining and holding your breath (Valsalva maneuver), can increase intra-abdominal and venous pressure.
- Exercises with Prolonged Standing: Activities that involve standing still for long periods can hinder venous return.
- Activities with a High Risk of Falling or Injury: This is crucial due to the increased bleeding risk from anticoagulant medication.
Managing Blood Clots and Blood Clot Leg Treatment
The overall strategy for managing blood clots involves several key components, with exercise playing a supporting role.
Anticoagulant Therapy
This is the mainstay of DVT blood clot treatment. Medications like heparin, warfarin, or newer oral anticoagulants (NOACs) are prescribed to prevent the clot from growing and to stop new clots from forming. This therapy is crucial for allowing the body to gradually dissolve the existing clot.
Compression Therapy
Wearing graduated compression stockings is a common and effective part of blood clot leg treatment and post-clot leg care.
- How it Works: These stockings apply gentle pressure to the legs, increasing venous blood flow and reducing swelling.
- When to Wear: They are often recommended during the day, especially when active, and can help prevent or reduce symptoms of post-thrombotic syndrome.
Lifestyle Modifications for Blood Clot Prevention
Beyond active treatment, adopting a healthier lifestyle is key for blood clot prevention.
- Regular Movement: Avoid prolonged sitting or standing. Get up and move around at least every hour.
- Healthy Weight: Maintaining a healthy weight reduces pressure on your veins.
- Smoking Cessation: Smoking damages blood vessels and increases clotting risk.
- Hydration: Staying well-hydrated helps keep blood from becoming too thick.
- Leg Elevation: Elevating your legs when resting can help improve circulation.
Physical Activity After Blood Clot: Long-Term Considerations
Recovering from a blood clot is a journey, and physical activity plays a vital role in the long term.
Gradual Reintroduction to Exercise
Once your doctor gives the green light, gradually reintroduce yourself to more vigorous activities.
- Listen to Your Body: Continue to monitor for any returning symptoms.
- Increase Intensity Slowly: Don’t rush back into your pre-DVT routine.
- Stay Consistent: Regular physical activity is the best long-term strategy for vein health and overall well-being.
Managing Post-Clot Leg Care
Long-term care after a blood clot often involves managing potential residual effects.
- Compression Garments: Continue wearing compression stockings as advised by your doctor.
- Regular Check-ups: Attend all follow-up appointments to monitor your vascular health.
- Healthy Lifestyle: Maintain all the lifestyle modifications mentioned earlier for ongoing blood clot prevention.
Table: Exercise Safety Checklist for DVT Patients
| Factor | Considerations | Action Required |
|---|---|---|
| Doctor’s Approval | Crucial before starting any exercise program. | Always get explicit permission from your physician. Discuss your exercise plan in detail. |
| Type of Exercise | Low-impact activities are generally safer. | Prioritize walking, cycling, swimming, and gentle yoga. |
| Intensity | Moderate intensity is usually recommended; avoid overexertion. | Start gently. Use the “talk test” – you should be able to talk but not sing during exercise. |
| Duration | Begin with shorter sessions and gradually increase. | Start with 10-15 minutes, build up over weeks. |
| Frequency | Regular, consistent activity is beneficial. | Aim for most days of the week, as advised by your doctor. |
| Symptoms Monitoring | Be vigilant for any signs of DVT recurrence or complications. | Immediately stop exercising and contact your doctor if you experience increased leg pain, swelling, redness, warmth, or shortness of breath. |
| Hydration | Dehydration can affect blood viscosity. | Drink plenty of water before, during, and after exercise. |
| Anticoagulant Meds | Increased risk of bleeding with injury. | Avoid activities with a high risk of falls or collisions. Report any unusual bruising or bleeding to your doctor. |
| Compression | Compression stockings can aid circulation and reduce swelling. | Wear prescribed compression stockings during exercise as recommended by your healthcare provider. |
| Warm-up & Cool-down | Prepares the body for exercise and aids recovery. | Include gentle stretching and slow movement for 5-10 minutes before and after your main exercise session. |
Frequently Asked Questions (FAQ)
Can I walk with a blood clot in my leg?
Yes, walking is often recommended for individuals with a blood clot in their leg, as it can help improve circulation and reduce the risk of complications. However, it’s essential to get your doctor’s approval first and start with short, slow walks, gradually increasing the duration and pace as tolerated.
What are the symptoms of a blood clot in the leg that I should be aware of?
Key symptoms of a blood clot in the leg (DVT) include swelling in one leg, pain or tenderness that may feel like cramping or soreness, redness or discoloration of the skin, and warmth in the affected leg. Leg pain that worsens when standing or walking is also a common sign.
Is it safe to exercise after having a blood clot?
Yes, physical activity is generally safe and encouraged after having a blood clot, once you have received clearance from your healthcare provider. The key is a gradual return to exercise, focusing on low-impact activities and listening to your body.
What is blood clot leg treatment?
Blood clot leg treatment typically involves anticoagulant medication (blood thinners) to prevent the clot from growing and new clots from forming. Other treatments may include compression stockings to improve circulation and reduce swelling, and in some cases, medication to dissolve the clot or procedures to remove it.
How can I prevent blood clots?
Blood clot prevention involves regular movement to avoid prolonged immobility, maintaining a healthy weight, not smoking, staying well-hydrated, and following any specific medical advice if you have a higher risk.
What is post-clot leg care?
Post-clot leg care focuses on managing any residual effects of the blood clot, such as swelling or pain, and preventing future clots. This often includes wearing compression stockings, regular exercise, and maintaining a healthy lifestyle.
Can I do strength training with a blood clot?
With your doctor’s approval, very light strength training can be incorporated gradually, focusing on controlled movements and avoiding heavy lifting or straining. Heavy weightlifting is generally discouraged, especially in the early stages, due to the risk of increased pressure and potential bleeding.
How long should I wait before exercising after a DVT diagnosis?
The waiting period varies depending on the individual’s condition, the location and size of the clot, and the prescribed treatment. It is crucial to consult your doctor for personalized advice on when it is safe to resume or begin exercising.
